Learn how glutamate impacts the brain, speech, behavior, and development, and why a low-glutamate diet may help kids with autism, childhood apraxia, or picky eating.
Early Intervention for Childhood Apraxia of Speech (CAS)
Is your toddler struggling with a speech-language delay? Do you suspect or have you wondered if your child may have Childhood Apraxia of Speech?
I was recently invited to be part of a blog collaboration about early intervention for Childhood Apraxia of Speech (CAS) by my friend and colleague, Tori Starling, CHHP. Tori is a holistic health practitioner, Documenting Hope Certified Health Coach, and Energy4Life bioenergetics practitioner. She is the founder of Simply Holistic Solutions, and the author of the novel Crazy Free & the non-fiction book Voice of Truth: A Mother’s Journey to Help Her Son Heal from Apraxia of Speech.
Twelve years ago, Tori helped her youngest son overcome Childhood Apraxia of Speech, eczema, and multiple food allergies. During that time, she created the blog, Jake’s Journey with Apraxia, which ran with the help of 19 other contributing writers for almost five years. As her son's health improved, she began to formally study natural health and energy medicine. She now helps moms of children with CAS take a holistic approach that addresses root causes and supports gut and brain health with the intent of making therapy with their Speech-Language Pathologist (SLP) more effective.
Please note some of my responses in the full blog collaboration were abbreviated for brevity and to best suite the flow of the collaborative blog. Below you’ll find my full responses to her prompts, but I highly encourage you to also visit Tori’s site for the complete blog post that includes additional dialog from Tori and fellow SLP, Katie Grecco. [Click here] to read the full blog collaboration.
“Big Pain Point: Parents suspect Childhood Apraxia of Speech (CAS) at 18-24 months old, but struggle with uncertainty because SLPs don't want to diagnose until age 3. This waiting period is frustrating and overwhelming.
I wondered this too when Jake was under 3. Why did he do basic speech therapy if apraxia was suspected?”
I can't speak specifically to Jake's experience because I wasn't his Speech-Language Pathologist (SLP), but I will say that most SLPs are not diagnosing Childhood Apraxia of Speech (CAS) before age 3 because it's difficult at that age to differentiate between CAS and other speech-language disorders that present similarly at that age. It is especially difficult to differentiate and identify if it's CAS when a child is younger than 3 years old, has less than 50 words, and/or is not combining words yet.
In my experience, some parents believe their child has CAS because of what they've found online but they don't have the full background knowledge and experience that SLPs do to differentiate between CAS and other speech-language disorders. There are a number of reasons and types of speech-language disorders that can be responsible for a child's delayed speech and language. A diagnosis of CAS requires that they meet all criteria for that specific diagnosis and when a child is younger than 3 (especially when they are using less than 50 verbal words), there are still too many unknowns to confirm a CAS diagnosis. At that point when they're younger than 3, SLPs could say that CAS cannot be ruled out and/or that the child is having difficulties with motor planning for speech, which may later qualify for CAS after age 3.
All of that being said, in many cases a skilled SLP can identify whether the child is experiencing a motor speech issue in the 18-24 month range (as long as the child is using enough verbal speech to assess their motor movements and speech patterns). It's important to see CAS as one of the diagnoses under an umbrella of motor speech disorders, understanding there are more motor speech disorders than just CAS that a child may have (like dysarthria for example, which can look similar to CAS under age 3, especially when a child is using very few words). The specific diagnosis becomes more important as the child grows older because the therapeutic approach should shift as they mature and have more capacity for more intensive speech-language therapies and approaches.
It's also important to note that some children with CAS also have Whole-body Apraxia or a Developmental Coordination Disorder, informally known as dyspraxia. When this is the case and you can clearly see that the child has difficulty with motor planning throughout their body, for gross and fine motor movements overall, not just for speech. In these cases when the child is younger than 3, we need to zoom out and focus on supporting coordination of the whole-body and gross motor movements before focusing intensely on motor planning for speech.
“What would it hurt to go ahead and start with apraxia therapy like DTTC, Kaufman, or PROMPT?”
It's very nuanced! These approaches are excellent for children with diagnosed CAS, especially school-aged children, in conjunction with other diet, nutrition, lifestyle and therapeutic supports. While these therapies are often recommended for children with CAS, they are applicable and supportive for children who have motor speech disorders, which CAS falls under the umbrella of. In my clinical opinion and experience, whenever a child is struggling with what appears to be a motor speech disorder, multimodal / multi-sensory cueing techniques and hierarchies (auditory, visual, tactile) should be utilized for support, regardless of age and if there's a diagnosis of CAS.
That being said, some of these approaches in their pure forms can sometimes be too much or too intensive for some children, especially for very young children which is why they aren't the default for most Early Intervention SLPs. When I was an Early Intervention SLP working with children younger than 3, I incorporated techniques from these motor speech-based approaches and blended multimodal cueing hierarchies into my child-led, play-based therapy sessions. Before age 3, therapy really should be child-led and family-centered vs. drill based therapies or other intensive types of motor speech-based therapies. You don't want to lose a kid in the therapy session, it's all about maintaining rapport. You have to "meet them where they are", but that doesn't mean that a skilled SLP can't or shouldn't be utilizing all of the tools in their toolkit when they see that the kiddo is struggling with motor planning for speech.
“What can a parent do while waiting for a diagnosis where they don't feel like they are wasting valuable early intervention time?”
I love this question because there's so much that parents can do to support their children at home! My suggestion is to not wait for a diagnosis to get started with speech-language therapy alongside diet, nutrition, and lifestyle changes, in addition to integrative therapies and modalities.
While there's no major issue in assuming your child may have CAS while waiting for an official diagnosis, it's important to have them formally assessed by an SLP to determine if the speech-language disorder is truly CAS and/or another speech-language condition. If they're younger than age 3, adjust your expectations accordingly knowing that you may not get a formal CAS diagnosis until then, however, that doesn't mean you shouldn’t pursue or continue speech-language therapy until you're able to get that diagnosis. It is common that children with CAS also have co-occurring language-based challenges that can be greatly supported by early intervention with an SLP.
Rather than focusing so much on the diagnosis during those early years, focus on the tailoring the approach to meet your child's needs, whatever that looks like for them. During this time, kids need the foundational supports in place before starting more intensive speech-language therapies for CAS anyways. I've found that these children benefit tremendously from nervous system supporting strategies and modalities, including movement-based therapies (ex: reflex integration and neurodevelopmental movement) as well as diet changes, targeted nutrition, and lifestyle changes to lower their "total load". Anything that can be done to support the child's nervous system, especially younger than age 3, can be really transformative in addition to therapy with a skilled SLP. Other examples for nervous system supportive therapies could be craniosacral therapy, Craniosacral Fascial Therapy (CFT), and/or nervous system focused chiropractic care (I love the PxDocs network for this type of chiropractic work).
One of the challenges with CAS and other motor planning conditions is that the terms that have been used to describe these disorders in the literature have been inconsistent, with changing diagnostic labels over time and differences in diagnostic labels depending on location. While not all children with CAS will have motor planning issues in their entire body, some do. Keep in mind that the movements of speech production are our finest fine motor movements that we use, and development builds onto development.
We develop gross motor skills before we develop and master fine motor skills, so it can be supportive to focus on the whole body and gross motor movements then fine motor with hands, all indirectly working to support fine motor with speech. Again, this is dependent on the child but if I were personally working with a child who I could see was struggling with coordinating motor planning of their whole body, I would incorporate whole body motor planning strategies into my session (and if needed, refer to an Occupational Therapist or Physical Therapist for support).
Diet and bio-individualized nutrition also supports the child's overall health, wellness, development and of course, their central nervous system regulation. While there isn't a large body of research looking at diet, nutrition, and CAS, there is some research that exists, in addition to growing body of anecdotal evidence from families, like Tori and Jake's story. There are more and more case reports coming out all the time about individuals (both children and adults) whose motor planning disorders improved when they changed their diet, especially the removal of gluten containing foods, and improving the gut-brain connection.
As an SLP and a Functional Nutritional Therapy Practitioner (FNTP), if I personally had a child who was suspected to have CAS and was in the 18-24 month range waiting for formal CAS diagnosis, here are a few things I would do (this list is hypothetical and non-exhaustive):
I would "clean up" their diet by removing artificial colors/dyes, artificial ingredients, GMOs, gluten, dairy, corn, and soy and focus on supporting their gut-brain connection. Additionally, I would assess if there are any nutritional deficiencies that could be playing a role (Vitamin E and Omega-3s for example) and address deficiencies with targeted supplementation as needed.
I would be intentional about letting my child get plenty of time outside daily, getting lots of movement and "heavy work" for regulation (bonus if they're barefoot).
In addition to speech-language therapy utilizing multimodal hierarchies and motor planning for speech strategies, I would enroll them in therapies that support nervous system regulation, starting with reflex integration and/or pediatric neurological focused chiropractic care.
I would also be very mindful to drop down to my child's level whenever possible so that we're face-to-face, so that they feel seen and heard while struggling to get their words out and so that they can see my mouth movements clearly. Try your best not to talk for your child or complete their sentences while they're attempting them with you, stay patient, model the correct form back to them once they've said it.
Regardless of whether or not your child has been formally diagnosed with CAS, at the 18-24 month stage, an SLP can and should be supporting parents with developmental strategies that they should be using at home to support their child's overall speech-language development. Ex: For 10-20 minutes a day (more if you can but do whatever you can fit in daily), get down on the floor with your child and let them lead the play. Follow their lead, use minimal language, and repeat the words or phrases they've said back to them with clear and exaggerated speech modeling. Get them looking at your mouth by placing toys near your face, don't withhold anything from your child making them "work" for it with their speech (that's a quick road to shut down and self-esteem issues). There are so many strategies that parents can use at home to support their kid, while waiting for diagnosis.
Again, it's all nuanced. The key is meeting your child where they are, always. While SLPs are a wonderful resource it's important note that not all SLPs are created equal and on the same page. Find someone who you can see building a great rapport with you and your child, and ask if / how they're using motor speech-based strategies and/or multimodal cueing hierarchies in their sessions (even when they're play-based, child-led, and family-centered).
I hope this has been supportive and gives you, the reader and presumably the parent, a sense of direction. I'm wishing your child and family all the best!
-
Once again, I would like to thank Tori Starling for the invitation to collaborate on this very important topic! If you’re interested in reading the full blog collaboration, learning more or connecting with Tori, please visit: simplyhealthsolutions.com.
If your child is struggling with a speech-language delay, you can also learn more tips and strategies to support them in my free podcast episode, Three Skills All Kids Need Before Developing Language: "Prelinguistic Skills" (S1 | 13). You can listen directly on the site by clicking below and/or on iTunes, Spotify, and other major podcast platforms.
Shandy Laskey, M.A., CCC-SLP, FNTP
Founder + CEO, Speaking of Health & Wellness, LLC
Healthier Halloween Ideas Your Kids Will Love!
Five Nutrients for a Healthy Brain & Which Foods to Find Them in
As the title shares, Episode 12 covers 5 nutrients for a healthy brain, not just for development and but also for general brain health! I share which foods to find these nutrients in and a variety of ways to incorporate these whole foods into your child's diet. I’m sharing insights and creative ways to improve your child's willingness to tolerate and try these new or even non-preferred foods. Hope you enjoy it!
Mentioned in the show:
Michelle Hoover from Unboundwellness.com - GFCF (AIP) Recipes - Salmon Cakes
Tony Mitra's work regarding organic chickpeas in North America containing glyphosate
Traumatic Brain Injuries, Leaky Brain-Leaky Gut, and Picky Eating...What's the Connection?
You may have heard of "leaky gut - leaky brain" but have you heard it the other way around? "Leaky brain- Leaky gut"?
In this episode, we're covering "leaky brain - leaky gut", primary and secondary brain injuries, a brief overview of the nervous system and the gut-brain connection, as well as the biochemical and neurobiological ways that complex picky eating can develop following a traumatic brain injury or even after a concussion that doesn't seem too significant or traumatic in nature.
We'll explore some beginning nutrition and lifestyle tips and strategies you may want to consider, regardless of how long it's been since the traumatic brain injury took place (although, the sooner the better of course). We'll cover how and why individuals with TBIs develop food and environmental sensitivities and what you can do to help support them, especially when it comes to complex picky eating.
If you're brand new to these topics of "gut health" and the gut brain connection, please visit Episode 6 titled, "How "Gut Health" Impacts Your Child's Health and Development" and then come back to this one. Episodes 6-10 are absolutely relevant to listen into if this resonates with you!
Do you know someone who could benefit from this information?
Please help spread this information to those who need it most by sharing this episode with them. Thank you so much for helping Speaking of Health & Wellness support more families and providers!
Enjoy the episode!
Could Your Child’s Physical and Behavioral Symptoms Be Caused By the Food They’re Eating?
Could your child’s physical and behavioral symptoms be caused by the food they’re eating? There are a number of ways that foods can impact children's health, physically and bio-behaviorally.
If your child struggles with complex picky eating, this one is for you!
If your child has developmental delays or a known neurodevelopmental condition, like autism spectrum disorders, ADHDs, speech-language disorders, sensory processing disorders, etc. then this one is for you!
If your child is struggling with a host of chronic health issue symptoms, this one is for you!
Did you know that over half of American children and millennials today have a diagnosable chronic health issue? Food and environmental reactions are very much involved here...
In this episode, I'm sharing an overview of the difference between food allergies, food sensitivities, and food intolerances. We'll cover the most common food allergies and sensitivities, as well as what physical and behavioral symptoms are seen in children with food reactions.
I share what to do if you think your child is experiencing negative reactions to their foods, starting with "cleaning up the diet overall", then navigating food sensitivity testing, and guidance around food elimination/reintroduction diets for food reactions.
Enjoy the episode! I hope that it's insightful and supportive for where you are on your journey!
Mentioned in the show:
Gluten Free, Casein Free Diets (GFCF) For Kids with Complex Picky Eating and/or Developmental Conditions - Answering FAQs
Episode 9 builds onto the information shared in previous episodes re: complex picky eating and neurodevelopmental delays and disorders being whole body conditions, as well as holistic nutrition, gut health, gluten free/casein free (GFCF) Diets... If you're new to the podcast and these topics, please go to earlier episodes in this Season 1.
I'm answering frequently asked questions that parents of these children often ask me when they're considering or starting the GFCF diet trial...
How do you know if they're getting or not getting the nutrients that they need? Can GFCF diets create deficiencies?
We specifically explore zinc and calcium and related factors to think about with these nutrients when implementing a GFCF diet.
Is the GFCF diet a lifelong change or temporary? How long until you see results? What would those results and improvements look like?
And lastly, I offer some guidelines and general habits for families to consider embracing during their transition to a GFCF diet with the child(ren) and/or family.
I'm answering all these questions and more. Enjoy the episode and don't forget to check out the resources linked below that I mention in the show!
Mentioned in the show:
My Accompanying Blog: "GFCF Diets, Picky Eating, Autism, & Other Neurodevelopmental Disorders...What's the Connection?"
Organic Olivia Herbal Supplements Line - For Kids & Adults - I use these products personally and with clients for support!
Is the Gluten Free, Casein Free Diet (GFCF) "All or Nothing?" What Happens if They Eat a Little Bit?
Episode 8 builds onto the information shared in previous episodes re: complex picky eating and neurodevelopmental delays and disorders being whole body conditions, as well as holistic nutrition, gut health, gluten free/casein free (GFCF) diets...If you're new to the podcast and these topics, please go to earlier episodes in this Season 1.
I'm answering frequently asked questions that parents often ask me when they're considering or starting the GFCF diet trial...
Is it "all or nothing?" What happens if they eat a little?
How long will it take to see results? What results could you expect to see?
Why do some people still say there's not enough evidence to support the GFCF Diet for these demographics of children and individuals?
What guidelines should be implemented to see the maximum benefit and potential of this transition, especially for families of children with complex picky eating?
I'm answering all these questions and more. I hope you enjoy the episode!
Mentioned in the show:
My Accompanying Blog: "GFCF Diets, Picky Eating, Autism, & Other Neurodevelopmental Disorders...What's the Connection?"
Organic Olivia Herbal Supplements Line - For Kids & Adults - I use these products personally and with clients for support!
GFCF Diets, Picky Eating, Autism, & Other Neurodevelopmental Disorders...What's the Connection? [Podcast]
We're covering the basics like what gluten and casein are exactly, the gluten free / casein free (GFCF) diet and exploring some of the research around it, as well as some thoughts you may want to consider before taking on a special diet for your child.
I'm covering 5 connections to consider when thinking about GFCF diets for children with complex picky eating, developmental delays, autism, and/or other neurodevelopmental conditions.
Mentioned in the show:
My accompanying blog: GFCF Diets, Picky Eating, Autism, & Other Neurodevelopmental Disorders...What's the Connection?
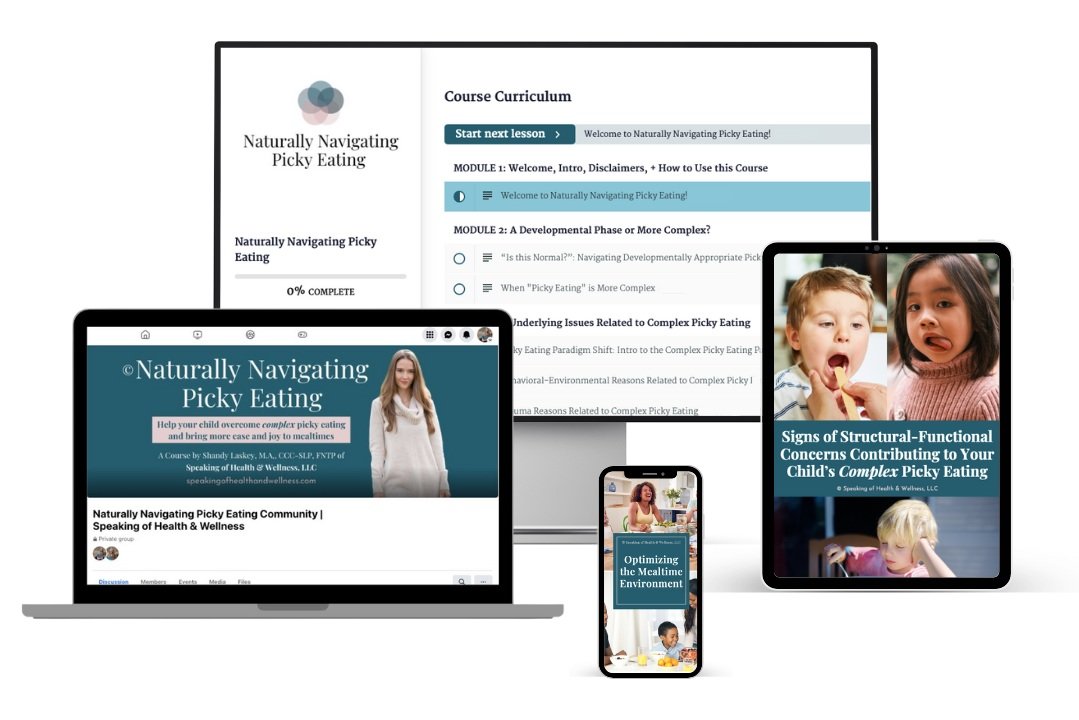
Are you ready to learn how to help your child overcome complex picky eating and bring more ease and joy to mealtimes?
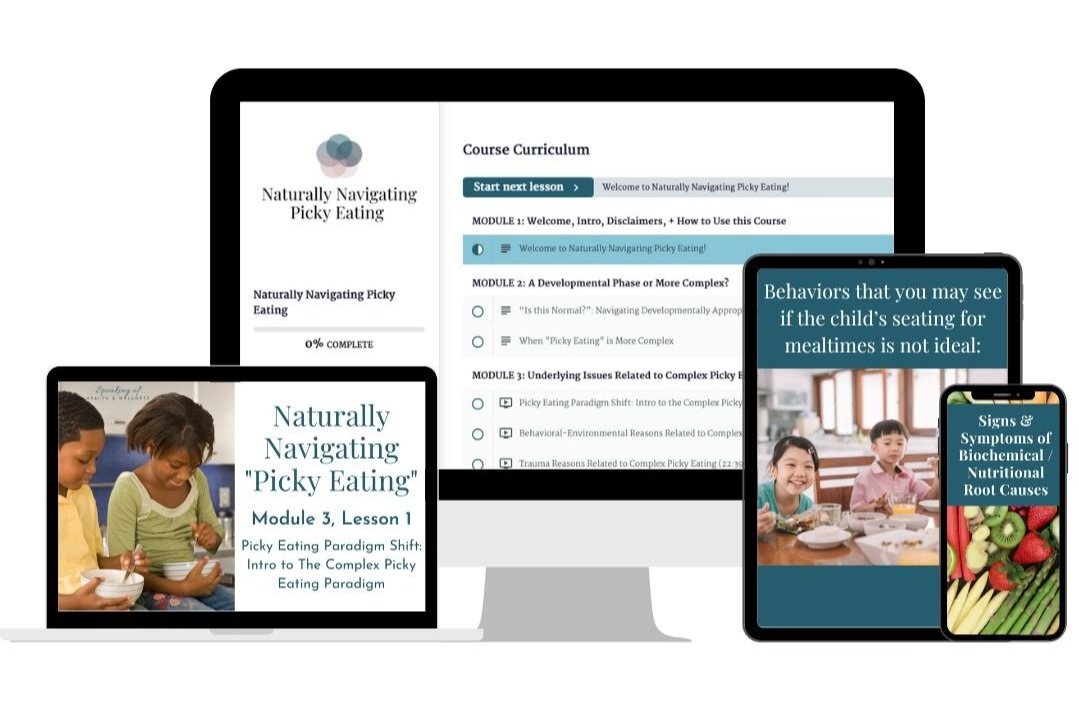
Enroll today in Naturally Navigating Picky Eating, a self-paced online course + guide for parents and caregivers of children with complex picky eating, with and without developmental conditions…
How "Gut Health" Impacts Your Child's Health and Development
"Gut Health", "The Gut-Brain Connection", "Gut-Brain Axis", etc. has been gaining more attention in the last decade, and understandably so! It's so important to our overall health and wellness, as well as children's development!
In this episode, I discuss some introductory terms that you'll hear when starting to learn more about gut health (microbiome, dysbiosis, leaky gut / intestinal hyper-permeability, etc.).
I share the signs, symptoms, and conditions that you may see when your child's gut health is in need of attention, as well as how gut health may be impacting children with complex picky eating, developmental delays, neurodevelopmental disorders, and more.
I hope you enjoy the episode!
Exploring Autism & Other Neurodevelopmental Disorders as Whole Body Conditions [Podcast]
The title says it all! In this episode we're exploring autism spectrum disorders and other neurodevelopmental disorders (like ADHD, childhood apraxia of speech, global developmental delays, etc.) as whole body conditions.
We're taking a closer look at the overlapping co-morbidities and the underlying root causes and symptoms these children and individuals share. I discuss the rise of these childhood disorders in tandem to the rise of chronic illness across the board in children and adults over the last few decades, and we talk about what beginning steps families can take towards living a more holistic and low tox lifestyle to support their child's health, wellness, and development.
Mentioned in the show:
My Accompanying Blog: Exploring Autism & Other Neurodevelopmental Disorders as Whole Body Conditions
My favorite low-tox cleaner for my home: Branch Basics (discount code included!)
Is Your Child's Picky Eating a Developmental Phase or a More Complex Issue?
Welcome to Episode 4, where I'm discussing “picky eating”. We're covering what's "normal" vs. what's not, and when to know if your child's picky eating is a typical stage of their development or if it's a more complex issue. I introduce my "Picky Eating Paradigm" and share some starting strategies for all children with picky eating that you can put into action right away! I hope you find this episode helpful and supportive!
Mentioned in the show:
Are you ready to learn how to help your child overcome complex picky eating and bring more ease and joy to mealtimes?
Enroll today in Naturally Navigating Picky Eating, a self-paced online course + guide for parents and caregivers of children with complex picky eating, with and without developmental conditions…
Holistic Nutrition & BioIndividuality: No "One-Size Fits All" Diet
We're exploring the concepts of holistic nutrition and bioindividuality. I discuss the various nutrition professionals and their titles, and how varying nutrition paradigms and views exist. Lastly, we'll cover the beginning steps that you can take to start your journey using holistic nutrition to support you and your family's health and wellness. Enjoy!